1st PUC Biology Question and Answer: Breathing and Exchange of Gases
Looking for 1st PUC Biology textbook answers? You can download Chapter 17: Breathing and Exchange of Gases Questions and Answers PDF, Notes, and Summary here. 1st PUC Biology solutions follow the Karnataka State Board Syllabus, making it easier for students to revise and score higher in exams.
Karnataka 1st PUC Biology Textbook Answers—Reflections Chapter 17
Breathing and Exchange of Gases Questions and Answers, Notes, and Summary
1st PUC Biology Chapter 17
Breathing and Exchange of Gases
Scroll Down to Download Breathing and Exchange of Gases PDF
Question and Answer:
Question 1.
Define vital capacity. What is its significance?
Answer:
Vital Capacity (VC): It is the maximum volume of air a person can breathe in after a forced expiration. This includes Expiratory Reserve Volume (ERV), Tidal Volume (TV), and Inspiratory Reserve Volume (IRV) — or the maximum volume of air a person can breathe out after a forced inspiration.
Significance:
It represents the maximum amount of air one can renew in the respiratory system during a single respiration. The greater the vital capacity, the more energy is available to the body for performing strenuous work. Vital capacity is generally higher in athletes and mountain dwellers, and young persons have more vital capacity compared to children or older individuals.
Question 2.
State the volume of air remaining in the lungs after a normal breathing.
Answer:
Functional Residual Capacity (FRC).
Question 3.
Diffusion of gases occurs in the alveolar region only and not in the other parts of respiratory system. Why?
Answer:
Only the alveolar region is made up of thin squamous epithelium and is richly supplied with blood capillaries, which makes it favorable for the diffusion of gases. The other parts of the respiratory system have thick walls meant for the conduction of air, not for gas exchange.
Question 4.
What are the major transport mechanisms for CO₂? Explain.
Answer:
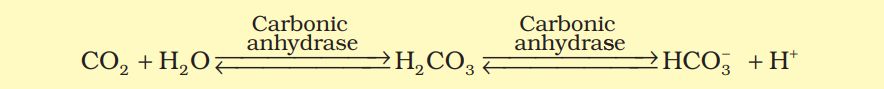
CO₂ is carried by haemoglobin as carbamino-haemoglobin. This binding is related to the partial pressure of CO₂. When PO₂ is low (as in the tissues) and PCO₂ is high, more carbon dioxide binding occurs, whereas when PCO₂ is low and PO₂ is high (as in the alveoli), dissociation of CO₂ from carbamino-haemoglobin takes place.
RBCs contain a high concentration of the enzyme carbonic anhydrase, which converts carbon dioxide to bicarbonates and vice versa. CO₂ diffuses into the blood and forms bicarbonate ions, thus CO₂ is trapped as bicarbonate at the tissue level and transported to the alveoli where it is released as CO₂.
A small amount of CO₂ also dissolves in plasma water and forms carbonic acid. On reaching the lungs, carbonic acid dissociates to release carbon dioxide.
Question 5.
What will be the po, and PCO, in the atmospheric air compared to those in the alveolar air?
(i) PO, lesser, PCO, higher
(ii) PO, higher, PCO, lesser
(iii) po, higher, PCO, higher
(iv) PO, lesser, PCO, lesser
Answer:
(1) Where there is low pO2 high pCO2, high H+ concentration and higher temperature exist, the conditions are favorable for dissociation of oxygen from the oxyhemoglobin.
(2) Where there is high pO2, low pCO2, lesser H+ concentration, and lesser temperature, the factors are all favorable for the formation of oxyhemoglobin whereas in the tissues.
(3) When pCO2, is high and pO2. is low as in the tissues, more binding of carbon dioxide occurs whereas.
(4) When the pCO2, is low and pO2, is high as in the alveoli, dissociation of CO2 from carbamino-hemoglobin takes place, i.e., CO2, which is bound to hemoglobin from the tissues is delivered at the alveoli.
Question 6.
Explain the process of inspiration under normal conditions.
Answer:
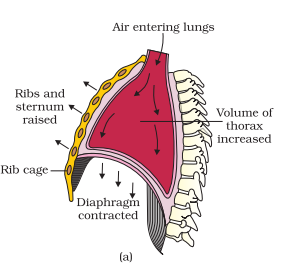
Inspiration occurs when the pressure within the lungs (intra-pulmonary pressure) is less than the atmospheric pressure, creating a negative pressure in the lungs.
- It begins with the contraction of the diaphragm, which increases the thoracic cavity volume in the antero-posterior axis.
- Simultaneously, external intercostal muscles contract, lifting the ribs and sternum, increasing the thoracic volume in the dorso-ventral axis.
- The overall increase in thoracic volume leads to a corresponding increase in pulmonary volume.
- This reduces the intra-pulmonary pressure below atmospheric pressure, causing air to flow into the lungs, i.e., inspiration.
Question 7.
How is respiration regulated?
Answer:
Respiration is primarily regulated by the respiratory rhythm centre in the medulla oblongata, which controls the basic breathing pattern.
- The pneumotaxic centre in the pons can shorten the duration of inspiration, thereby adjusting the respiratory rate.
- A chemosensitive area near the rhythm centre detects increases in CO₂ and H⁺ in the blood and stimulates the rhythm centre to modify breathing accordingly.
- Peripheral receptors in the aortic arch and carotid arteries also sense changes in CO₂ and H⁺ levels and send signals to the brain to maintain proper respiration.
Question 8.
What is the effect of pCO, on oxygen transport?
Answer:
In the alveoli, where there is high PO₂, low PCO₂, low H⁺ concentration, and lower temperature, the conditions are favorable for the formation of oxyhaemoglobin. Whereas, in the tissues, where low PO₂, high PCO₂, high H⁺ concentration, and higher temperature exist, the conditions are favorable for the dissociation of oxygen from oxyhaemoglobin.
This indicates that O₂ binds to haemoglobin at the lungs and gets released at the tissues. Every 100 mL of oxygenated blood can deliver around 5 mL of O₂ to the tissues under normal physiological conditions.
Question 9.
What happens to the respiratory process in a man going up a hill?
Answer:
When a man goes uphill or does strenuous exercise, oxygen consumption increases, which decreases the partial pressure of oxygen in haemoglobin, creating a higher demand for oxygen. As a result, the breathing rate increases to supply sufficient oxygen to the body.
Question 10.
What is the site of gaseous exchange in an insect?
Answer:
Insects have a network of tracheal tubes that transport atmospheric air directly to the body cells, allowing the cells to exchange gases directly.
Question 11.
Define oxygen dissociation curve. Can you suggest any reason for its sigmoidal pattern?
Answer:
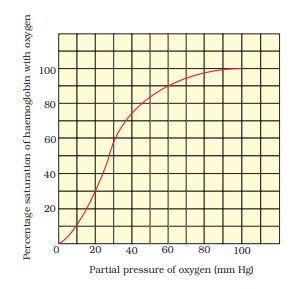
Oxygen dissociation curve: It is a graphical representation of the relationship between the partial pressure of oxygen (PO₂) and the percentage saturation of haemoglobin with oxygen.
The graph is sigmoidal (S-shaped) because:
- At low PO₂, the formation of oxyhaemoglobin is slow, so the percentage saturation is low.
- As PO₂ increases, haemoglobin binds oxygen more readily, and the percentage of oxyhaemoglobin rises steeply.
- When PO₂ reaches around 100 mm Hg, haemoglobin becomes fully saturated, and a further increase in PO₂ does not increase saturation, resulting in the plateau of the curve.
Question 12.
Have you heard about hypoxia? Try to gather information about it, and discuss it with your friends.
Answer:
Hypoxia refers to a shortage of oxygen supply to the body. It can occur in different forms:
- Anemic hypoxia: Caused by deficiency of haemoglobin.
- Cytotoxic hypoxia: Due to impaired oxygen utilization by cells, as in cyanide poisoning.
- Stagnant hypoxia: Caused by poor blood circulation, e.g., in heart failure.
- Hypoxic hypoxia: Due to insufficient oxygen in the air, e.g., at high altitudes.
- CO poisoning: Carbon monoxide binds irreversibly to haemoglobin, reducing oxygen transport.
Question 13.
Distinguish between
(a) IRV and ERV
(b) Inspiratory capacity and Expiratory capacity.
(c) Vital capacity and Total lung capacity.
Answer:
(a) IRV and ERV
- Inspiratory Reserve Volume (IRV): Additional air a person can inhale forcibly after a normal inspiration (≈ 2500–3000 mL).
- Expiratory Reserve Volume (ERV): Additional air a person can exhale forcibly after a normal expiration (≈ 1000–1100 mL).
(b) Inspiratory Capacity and Expiratory Capacity
- Inspiratory Capacity (IC): Total air a person can inhale after normal expiration; equal to TV + IRV.
- Expiratory Capacity (EC): Total air a person can exhale after normal inspiration; equal to TV + ERV.
(c) Vital Capacity and Total Lung Capacity
- Vital Capacity (VC): Maximum air a person can breathe in after forced expiration or breathe out after forced inspiration; sum of TV + IRV + ERV.
- Total Lung Capacity (TLC): Total volume of air lungs can hold at the end of forced inspiration; sum of VC + Residual Volume (RV) or TV + IRV + ERV + RV.
Question 14.
What is Tidal volume? Find out the Tidal volume (approximate value) for a healthy human in an hour.
Answer:
Tidal Volume (TV): The volume of air inhaled or exhaled during normal respiration. It is approximately 500 mL.
- Breathing rate: 12–16 breaths per minute
- Tidal volume per minute: 500 × 12–16 = 6000–8000 mL (6–8 L)
- Tidal volume per hour: 6–8 × 60 = 360–480 L
ADDITIONAL QUESTIONS AND ANSWERS
Question 1:
What is the difference between conducting part and respiratory part of the human respiratory system?
Answer:
- Conducting part: Includes nostrils, nasal cavity, pharynx, larynx, trachea, bronchi, and bronchioles. It transports, filters, warms, and humidifies air.
- Respiratory part: Includes alveoli and alveolar ducts. It is the site of actual gas exchange between air and blood.
Question 2:
What is the role of pleural fluid in the lungs?
Answer:
Pleural fluid is present between the two layers of pleura. It reduces friction during breathing movements and allows smooth expansion and contraction of the lungs.
Question 3:
Explain cutaneous respiration in amphibians.
Answer:
Amphibians like frogs can exchange gases through their moist skin. Oxygen diffuses in and carbon dioxide diffuses out. This is supplementary to lung respiration and is called cutaneous respiration.
Question 4:
Define residual volume and its importance.
Answer:
Residual volume (RV): The volume of air remaining in the lungs after a forced expiration, averaging 1100–1200 mL.
Importance: Prevents lung collapse and maintains continuous gas exchange even between breaths.
Question 5:
What is the role of carbonic anhydrase in CO₂ transport?
Answer:
Carbonic anhydrase is an enzyme in RBCs that converts CO₂ and H₂O into carbonic acid (H₂CO₃) and vice versa. It facilitates CO₂ transport as bicarbonate ions from tissues to alveoli, where it is released as CO₂.
Question 6:
What are partial pressures of gases and how do they influence gas exchange?
Answer:
Partial pressure is the pressure contributed by a specific gas in a mixture. Oxygen diffuses from high PO₂ in alveoli to low PO₂ in blood, and CO₂ diffuses from high PCO₂ in blood to low PCO₂ in alveoli. It is the main driving force for diffusion.
Question 7:
Why is CO₂ more soluble than O₂ in blood? What is its significance?
Answer:
CO₂ is 20–25 times more soluble in plasma than O₂.
Significance: Even with smaller partial pressure differences, CO₂ diffuses easily from tissues to blood and from blood to alveoli for elimination.